Ping. That must be my daily reminder. How am I feeling now in terms of arousal and valence? Well, I just had my weekly meeting with my research advisor. He was really getting into the nitty-gritty and suggested that I should have been farther along with my project. I don’t even like this project. I wish I could just get it over with… Anyway, probably low valence. It was a pretty negative experience. Also high arousal… He really stresses me out, and I could feel my blood pressure rising.
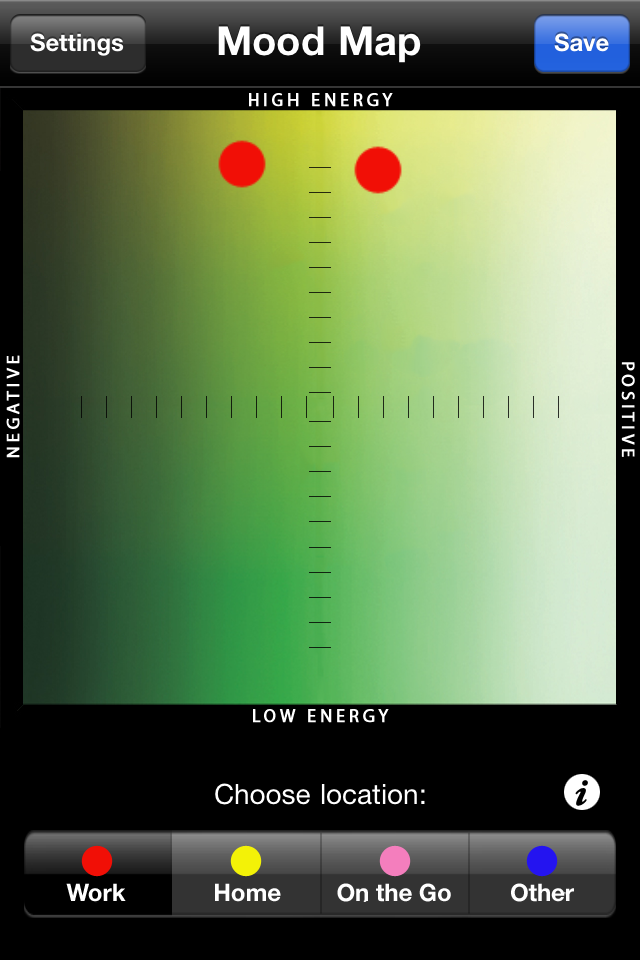
Photo Credit: mzstatic.com
One of the greatest benefits of mood tracking is increased self-awareness. Mood tracking apps like Moodscope and Mobile Therapy remind users to take a step back and to reevaluate their life choices. They can reflect on what is bringing them happiness and what is bringing them down. By connecting their moods with other factors happening in their lives, users can develop a greater understanding of themselves with respect to their environment.
The beauty of mood trackers is that they also provide spatial and temporal information. Users can link their moods to their immediate spatial surroundings and to the time of recording. By randomly sending pings throughout the week, these apps can help users determine where and when they tend to feel upset or happy.
Additionally, mood trackers do not only take in information, they can also offer advice. Mobile Therapy offers therapeutic exercises, including breathing visualization and muscle relaxation. It also offers strategies to quit smoking, treat anxiety, and detect relapses in psychotic disorders. Ideally, these mood tracking apps could personalize therapeutic exercises to a user’s specific input. You could “have it your way” by inputting end goals, such as cultivating happiness or controlling the relaxation response.
Photo Credit: play.google.com
With most mood trackers, it is also possible to add information through texting—users can share paragraphs of information if they feel inclined to do so. Therapists and physicians could use these self-reflections to see how their patients are doing over time. Appointments with health professionals are short, and they are not necessarily indicative of how the patient normally acts. Some patients may experience white coat syndrome, so there is an additional benefit of having records of patients outside of the doctor’s office.
In the future, perhaps these apps could notify the patient’s physician directly. Jon Cousins describes the benefits of connecting his data to those close to him: “We leave traces of ourselves with our numbers, like insects putting down a trail of pheromones, and in times of crisis, these signals can lead us to others who share our concerns and care enough to help.”
If physicians have access to their patients’ personal information, they can individualize their treatments. While there would be a lot of information to handle, this issue could be alleviated with efficient organization and clean programming. It is possible to automatically assemble the relevant information in a visually aesthetic way, and these apps track not only the physical health of users, but also their mental and psychosocial health.