Telehealth advocates the use of electronic services to support patient care, education, and monitoring. Proponents of telehealth acclaim its potential to reduce healthcare costs and to increase patient satisfaction. Implementing telehealth, however, would require deconstructing the traditional healthcare encounter. Patients and physicians would have to redefine their expectations for one another, and some argue that telehealth belittles the patient-physician relationship.

Photo Credit: firsthealth.org
Nevertheless, there are clear advantages for telehealth. Telehealth can serve as a means of supporting traditional healthcare. When distance separates participants, patients can use electronics to directly contact their physicians. They can receive direct clinical service miles away from the doctor’s office via virtual visits. If the patient’s health records, medical images, and medication lists are already compiled online, such virtual visits can serve as a timely and efficient way to improve patient care.
Additionally, telehealth allows the early detection of irregular or unfavorable body rhythms. For instance, early detection of irregular heart and brain rhythms could prevent potential heart attacks and seizures. In this respect, telehealth plays a role in preventive medicine and contributes to better health outcomes.
Schwamm (2014) gave an example that cellphone cameras could be used to photograph rashes and skin lesions. This would allow dermatologists to diagnose and treat their patients without having to physically meet. While this form of treatment is fast and efficient, it seems to be in stark contrast with integrative medicine.

Photo Credit: mc.vanderbilt.edu
Growing in favor since the 1990s, integrative medicine emphasizes a holistic approach to medicine with a focus on health and the physician-patient relationship. With this method of telehealth, the physician-patient relationship is almost nonexistent, and patients are reduced to their skin problems. Furthermore, diagnosis via photograph is hardly holistic; rashes and skin lesions may be signs of a multitude of health problems. It is unlikely that only the dermis is affected, and it would be erroneous to assume that the organ systems of the body work independently.
In Engel (1977)’s seminal article, he claimed the need for a new medical model—namely, the biopsychosocial model. This model posits that biological, psychological, and social factors all play a significant role in the context of disease and illness. Integrative medicine relies on this model because it focuses on the whole body. Therefore, it seems to be opponent to this localized method of diagnosis.
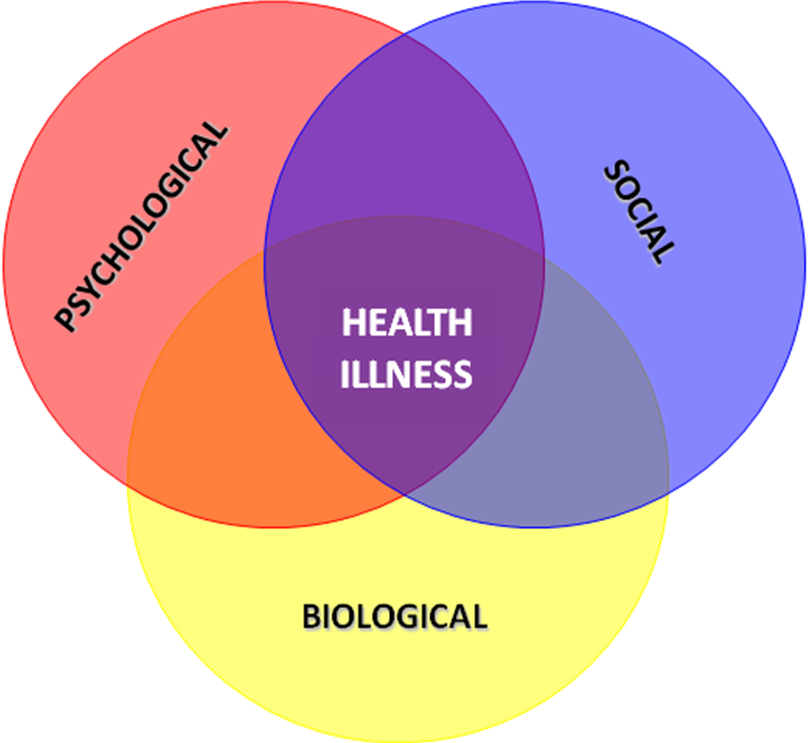
Photo Credit: theemotionmachine.com
While telehealth has its greatest benefits in early detection, it still has some outstanding limitations. In accordance with the biopsychosocial model, the physician also plays a role in helping the patient cope with stress and vulnerability. On a standardized stress scale, finding out that you are HIV+ scores a 99/100. Given current technological advances, it is possible to get tested for HIV without ever having to actually see a doctor; however, this is a questionable idea. Beyond biomedical treatment, the physician also provides intimate psychological and social support.
Currently, telehealth and integrative medicine can coexist; however, telehealth has its limitations. While it should complement and add value to existing medical care, it should not substitute healthcare completely.




