As Socrates once said, “to be is to do.”
As an aspiring physician, I’ll soon enter a clinical environment that’s more data-driven and technology-oriented than ever before. More patients are using mobile applications to track their health data. More providers are incorporating patient-generated big data into clinical decision-making. More devices are becoming integrated into the Internet of Things, a connected contextual framework with the power to drive personalized, predictive healthcare.
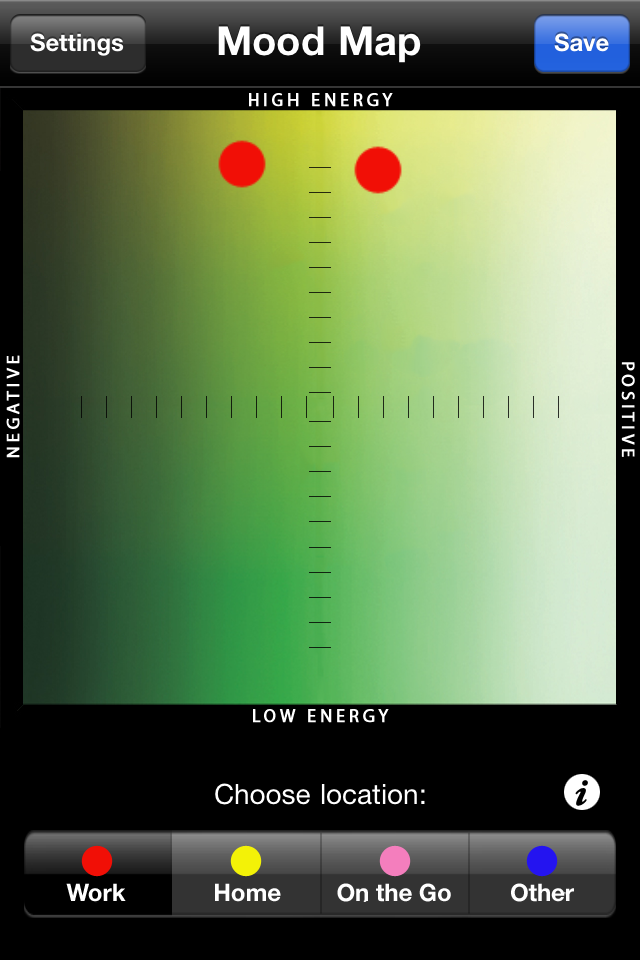
In class, we’ve discussed how e-patients can use self-tracking to build awareness and control over their health status. In our design setting, we’ve examined how intensive care physicians have to consolidate vast quantities of data into a cohesive patient narrative and a plan of care. But there’s discussing and observing, and then there’s doing. I decided to take it a step further. I wanted to situate myself in the patient’s, or provider’s perspective, using self-tracking to inform and inspire my own health behaviors.
Over the past 30 days, I’ve used Azumio’s Argus to construct a digital timeline of my lived experiences. Every morning, I log my sleep, heart rate, and blood pressure. As I walk across campus, I measure my steps and calorie consumption. When I sit down for a meal, I take a snapshot of my plate. With each meal, I record how many glasses of soda and/or water I’ve had. When I hit the Rec Center, I record my exercise by type and duration. If it’s a weeknight study session, I count how many cups of coffee or tea it takes to power through it. If it’s a weekend, as I hit the bars, I save how many bottles of beer or glasses of wine I’ve had. And at night, I check my pulse and blood pressure again right before my head hits the pillow.
Now, the critical question: what have I learned?
Commitment. Between Week 1 and Week 4, my “compliance” fell from 96% to 63%. It takes a committed, conscious effort to record every meal, every vital sign, every exercise, every minute of the day. I hold a new-found respect for the diabetic patient who has to monitor his blood sugar, manage his appointments, and mind his meals; it’s a process that’s both distracting and exhausting.
Awareness. As much as the constant inputs were a challenge, they empowered me to become cognizant of my daily behaviors. Did I really eat pizza and chips for lunch that often? I went that long without drinking water? Do I really spend so much of my day in a sedentary state? To record empowers us to know, and to know inspires us to act. I wonder if, as we move towards ‘ambient-tracking’ devices, we’ll lose this sense of awareness and agency.
Application. So often I found myself asking, what really matters? Argus would frequently warn me that I hadn’t drank water in three hours, or congratulate me for walking 10,000 steps that day. Did these things necessarily make me a healthier person? As we realize our ability to quantify everything, it’s important for us to isolate signals amidst noise. It’s necessary that we identify the parameters that matter for health versus those that don’t. It’s vital that we appropriately calibrate the thresholds of behavior that justify a congratulatory or cautionary alert. Data for data’s sake is useless; the next step is to make that data actionable.
If you haven’t quantified yourself yet, it’s a must. Data is a ubiquitous element of our modern lives. When we quantify ourselves, we can critically evaluate our daily experiences from a birds-eye vantage point. We can channel those insights into knowledge and action to enrich our lives. And, as future physicians, we can learn what it means to gather data, make sense of data, and use data to drive clinical decisions.