According to rumors, the newest version of the Apple OS system, iOS 8, will include an Apple-designed app called “Healthbook” that will be a “preinstalled app that can track data points including a user’s blood pressure, hydration, heart rate and potentially other statistics like glucose levels. It could also remind users to take medications at certain times during the day.” According to the description and concept art, Healthbook intends to be an all-in-one resource for all kinds of self-tracking, including dietary monitoring, fitness, filling prescription. It is not clear whether it intends to self-diagnose any diseases.
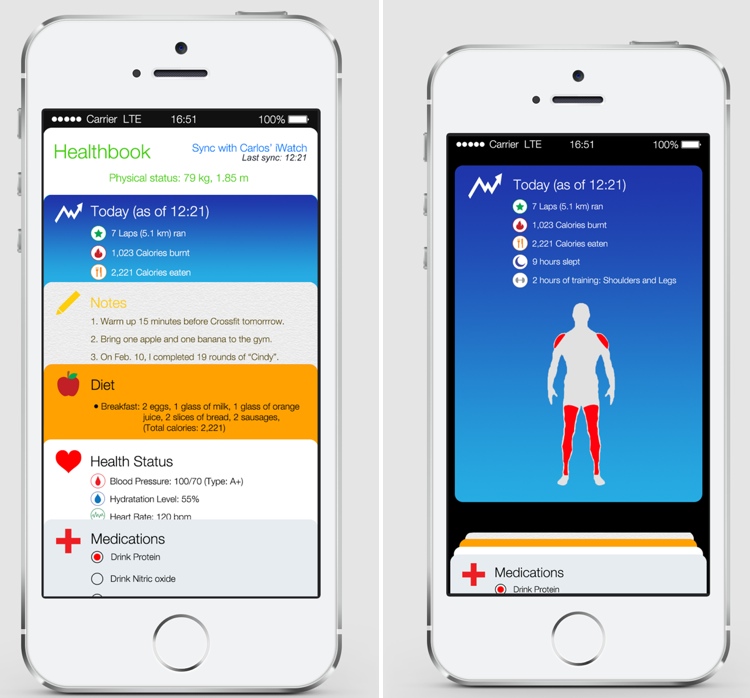
Concept images for the “Healthbook” iOS App, courtesy of MacRumors
iOS 8 is expected to be announced at Apple’s annual World Wide Developers Conference in June 2014. This means that Healthbook could become available as early as this fall. It is also predicted that the Healthbook App will also be integrated with the upcoming iWatch.
What will having a preinstalled application on such an widely accessible device like the iPhone mean for the healthcare movement, especially self-trackers? Although the app stores contains hundreds of thousands of health-related applications, will having an official Apple-designed healthcare mobile application increase a user’s proclivity to become an e-patient, self-tracker, or be more aware of their health? How will Healthbook take into consideration the major issues regarding self-tracking applications such as privacy and user control?
And what about Apple’s design strategy? What features or GUI aspects will differentiate it from other self-tracking applications in the App Store and on Android? Reports claim it will use a similar card-based design strategy similar to Passbook, another Apple-developed application that keeps all your forms of payment, such as credit cards, in one place and was meant to serve as a virtual wallet of sorts. Will having all your health data in one place be seen as efficient and beneficial, or dangerous in regards to privacy?
My guess? Healthbook will receive a lot of early hype and attention, especially as the release of iOS 8 draws closer, and upon official release many curious users and e-patients galore will use the application in its early stages. However, unless Healthbook provides some sort of dynamic, engaging experience beyond being a basic self-tracker application, users who are were not originally intrinsically motivated to monitor their health will become bored by it and eventually stop using it. As we have learned, most self-trackers are not those who are in need of medical attention, but those who already have an interest in maintaining their health, and unless Apple brings something new to the table with Healthbook, the average user will see Healthbook not as a life-saving tool, but a new toy or game, and will quickly become bored once it loses its novelty.
Here’s two suggestions for how Apple can distinguish Healthbook from its competitors and engage the interests of users who have not had previous interest in self-tracking their health lifestyles:
- For the dietary/calorie tracker, add fun facts to inform and put their diet into perspective. For example, if after a run a user burns 200 calories, Healthbook can joke “You just burned off a bag of chips”.
- Have a goal-setting feature that includes specific suggestions on how to achieve that goal. For example, if a user wanted to lose 10 pounds, Healthbook could not only suggest how many miles they should run a week, but also suggest dietary restrictions and specific workout routines the user can engage in to create a total body regime that will help reach the user’s goal.
Whether these features or something even better (as Apple’s forte is coming up with what the user needs before they even need it) will be included in the Healthbook application remains to be seen. I am personally very glad Apple is trying to create an accessible and beneficial device that could provide better awareness of personal health. Apple has reinvented the personal computer, music, cellphone, and tablet industries, and I hope it can achieve the same success in revolutionizing the mobile healthcare space.