http://sam-app.org.uk/
Category Archives: Technology
Increasing the Scope of mHealth: Telemedicine Behind Bars
In designing mHealth solutions, one of the most important initial steps is identifying the target population. Asking “Who will benefit?” is one of the best ways to kick-off a successful, targeted mHealth campaign. To do this, we spend time gathering statistics about how many people own mobile phones, who owns smartphones, who texts, who tweets, and who talks. As we narrow down our target population to a specific subset, certain groups will inevitably be left out. One such population, is the incarcerated.
While inmates are not generally allowed access to mobile phones, mobile health, specifically telemedicine, holds a lot of promise in improving healthcare among this population. In December 2013, mHealth News reported that the Louisiana Department of Corrections (DOC) was planning to increase the use of telemedicine in their prisons three-fold as the primary healthcare delivery system for its inmates. By collaborating with AMD Global Telemedicine Inc—the leading Telemedicine Encounter Management Solutions supplier—the DOC hopes to serve over 50,000 inmates. Prior to this innovation, handcuffed prisoners had to be transported 150 miles by bus to reach the nearest healthcare facility, where all prisoners had to remain until everyone had been seen.
By establishing a telemedicine infrastructure—training doctors and healthcare professionals and purchasing video and medical equipment—inmates can be screened for the few that need face-to-face interaction, while the others can be seen virtually from the prison. With the technology provided by AMD, up to 15 patients can be seen by a single physician in just four hours. In addition to increasing productivity and tailoring care, the increased use of telemedicine is also cost-effective. Using telemedicine will greatly reduce transportation costs and payment for personnel who need to be transported from the prison. Additionally, the DOC is receiving additional funding from the state, which will allow it to pay for the aforementioned training and purchases.
Telemedicine is also especially valuable because it provides an opportunity for the consolidation of medical information through the digital interface. An article in PRWEb covering this telehealth development describes the program’s capacity to “deliver live medical images from connected medical devices and scopes, real-time video from an examination camera, and the ability to view patient documents and vital signs data all in the same online platform.” Furthermore, patients can use telemedicine to access physicians of 16 different medical specialties, including primary care, neurology, and endocrinology.
Telemedicine provides a very promising avenue for using media and digital technology to reach underserved populations. The incarcerated community is oftentimes overlooked for many medical innovations. However, this is one valuable opportunity in which such innovations can, and most likely will, be both highly useful and significantly impactful. While it is simple enough to design media solutions for educated professionals, the potential of mHealth is much more expansive, and should be utilized in as many ways as possible.
http://www.mhealthnews.com/news/telemedicine-behind-bars-prison-mobile-mHealth?page=0
http://www.prweb.com/releases/2014/02/prweb11575342.htm
Developing SciFi: The Medical Tricorder
Have you heard of the medical Tricorder? It’s the fictional device used in the Star Trek universe to instantly diagnose disease without any invasive procedures. This space gadget seems like it could be pretty useful, but it isn’t real. Or is it?

In 2011, a non-profit organization focusing on technological development, X Prize, and the wireless telecommunication company, Qualcomm, organized the Qualcomm Tricorder Competition, inviting scientists world wide to turn the fictional medical Tricorder device into the next real health-tech breakthrough. The winner is to develop a hand held device that will diagnose patients better than or equal to a panel of board certified physicians.
The ultimate goal of this competition is to develop a device that will provide instantaneous medical feedback for an individual’s health status without any invasive procedures or trip to healthcare facilities. This, in theory, would give individuals direct access to health data as well as full control over how, when, and where they receive care.
This science fiction idea seems radical in that it is trying to condense the entire primary care physician’s job into one handheld device. With the development of devices such as the lab-on-a-chip, maybe the technology does exist that this device may not completely be out of reach. However, is it right to outsource such a huge task to a little phone screen? Even if such computerized devices give rise to better diagnostic outcomes than the 55% (as reported by the Qualcomm competition website) met by human physicians, is it right to shrink medicine down to statistics and algorithms?
Of course, even if this device is to be made, more invasive procedures will probably continue to be done in hospital – but that being said, I would like to believe that there is more to medicine than just providing a diagnosis. The new technology (again, in theory) will be able to gather health metrics to raise concerns for a specific diagnosis, but full patient context should be understood before making health decisions.
The medical tricorder may be perfected to be used as a supplementary medical device for those willing to purchase such a device – but this should never replace a doctor’s visit. The organizers for this competition provide the rationale that people more often than not must seek a healthcare professional in order to receive any type of direct medical care, creating an inefficient healthcare system that is out of reach for those who actually need it.

Although the concern brought up by the Qualcomm and X Prize is certainly valid, creating technology to replace doctors to an extent seems to be a bit extreme. Many studies have definitely shown evidence that increased physician-patient interaction correlate with better outcomes. Just from personal experience in research, I have seen the large positive placebo effect on patients just from being able to talk to a professional.

Patients who are going to the doctor out of concern for personal well-being are going to go to the doctor regardless of what a machine tells them. Those that are going to be persuaded not to go are those that probably wouldn’t have gone unless the symptoms were truly bothersome anyway – so in a sense – we aren’t really getting anywhere with this.
Sometimes, what the patient needs is genuine attention from the HCP, not an analysis of story-less numbers and figures. Technology can always be a great supplement, fulfilling biological human needs, but not enough to fulfill personal human needs.
A New Approach to Treating Mental Illnesses
While we often think of new applications of medical technology as having vast implications for the treatment of many diseases, mental illnesses are often left out the discussion. This exists due to the deeply ingrained stigma in our culture that mental illnesses are not “real” diseases. However recent advances in technology have had a large influence on addressing the stigma of mental illness and providing new treatment approaches for mental illnesses.
One of the greatest impacts of new technology on mental illnesses is creating an online forum where people feel comfortable discussing their illness and can connect with others who are living with the same illness. While technology enables this for a variety of illnesses, it is especially important for mental illnesses because people with a mental illness can often feel isolated and feel pressure to hide their illness. Reading the stories of others, who are facing the same type of struggles, can encourage someone to seek treatment. The information available online creates an open dialogue in which we all can become better educated on mental illness, which will hopefully begin to break down the stigma ingrained in our culture.
New advances in technology are also impacting the treatment for various mental illnesses. One particular multimedia program that is garnering attention is called Virtual Reality, and was developed for patients with Post Traumatic Stress Disorder. The program is based on exposure therapy, and uses specially programmed computers to create an artificial environment designed to be similar to scenarios a veteran experienced during combat. This program has also been shown to reduce a number of phobias, including arachnophobia, by having patients work their way through various scenarios that include their phobia, thus becoming more accustomed to their fear.
Future advances for the treatment of mental illnesses might involve applications that sense when a user’s mood is changing or if the user is in a high-risk situation. Mood could be tracked using physiological measures, and could signal a potential manic or depressed state. Location could be correlated to mood, and send a comforting or alerting message to the user if they are in an area where they normally experience high stress. For example, if a phone detects someone who has been diagnosed with depression with a predisposition towards alcoholism buying alcohol alone late at night, it could alert a family member to check on their loved one. While promising, these new features lead to many privacy and security concerns. Although it might seem easier to limit the app to solely the patient, allowing the patient’s family and friends to be part of the treatment plan is essential, especially for mental illnesses.
While technological innovations for the treatment of mental illness are advancing rapidly, the technology out there lags behind many other “typical” diseases. Hopefully, even more innovative treatment approaches will soon be created, creating a brighter future for the treatment of mental illnesses.
EMR vs. EHR: What does it really mean?
One of the topics that we have discussed on varying occasions throughout the semester is electronic health records (EHR) and how they interact with and effect patient care. In my own groups work with our problem owner in the CV ICU, interaction with the EHR has been a large part of developing a solution. As I have continued to work with and research the present systems, I have noticed, both in the classroom and in the hospital environment, an inconsistency in terminology used to refer to the records. From what I observed, the terms electronic medical record (EMR) and electronic health record (EHR) are often used interchangeably. Curious, I looked to see if there was an actual difference between these two records and how they are involved in medicine.
Google Trend Data Tabulating Searches for “EMR”and “EHR”
Though these terms are often used synonymously, there are marked differences between EHRs and EMRs and how they are used within the medical field. My research led me to discern that the term EMR refers to essentially a digital version of the paper charts that they replaced. These digitalized systems contain a patients medial and treatment history specific to a doctors practice and posses the ability to allow caretakers to track data over time, identify which patients are due for screenings or appointments, and monitor quality of care within the practice. The largest difficulty when using EMR is transfer of information out of a physicians practice, and in that sense does not improve significantly from a paper record.
So how do EHRs differ from what I have just described? The key difference between an EMR and EHR is the focus of use. As described by a variety of sources, an EHRs functional aim is to address the total health of the patient, going beyond the original health organization to encompass information from other health providers including laboratories, specialists, and most importantly the patients themselves. The ability to share information in a secureway throughout all aspects of patient care creates the possibility for interactive communication and the meaningful use of EHRs as a tool to improve patient care.
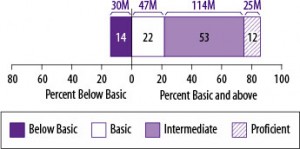
Overall, what I found is that while the terms EMR and EHR only differ by one word, that small change makes a world of difference. The engagement and commination opportunities that the EHR provides, makes a case for the use of these systems exclusively. A push for providers to engage patients through their access to the EHR system has occurred in recent years, but is this engagement really effectual and beneficial to patient care? With an estimated 77 million Americans that possess either basic or below basic health literacy, are EHR systems providing accessible and useable information to patients to improve their care or are many patients just getting lost in the process?
To answer that question the Agency for Healthcare Research and Quality have examined health education materials delivered by EHRs and have determined that many do not often account for the poor health literacy possessed by a large amount of the population. So what can we do to make EHR systems more useable for patients and improve care outcomes?
A number of leaders of Health IT have begun address this disparity by suggesting a list of preliminary standards and key tools designed to be incorporated into the existing and new EHR systems. A number of simple changes to improve direct communication with patients include providing patients with the ability to identify their preferred language. Other functions including the ability of EHRs to filter quality measures by patient characteristics such as language, socioeconomic status, and education level, could work to reveal and address disparities in care, including those involving health literacy. In addition to providing better resources for patients, having EHRs include information such as disability status, sexual orientation, or gender identity can provide caregiver a greater context regarding a patient’s health recommendations and outcomes. While these changes serve as the initial push in addressing functional and health literacy changes to EHRs, there are still ways to improve the educational value of the interactive system.
What other innovations could be incorporated into EHR systems in improve health literacy?