Over the last month, Team SAVE has conducted interviews with patients who have participated in or are currently participating in clinical trials. In each interview, we asked the patient about their experiences, opinions, and suggestions. While conducting these interviews, we noticed a common thread among what many of the patients said; in almost every interview that we have conducted thus far, the interviewee has said something along the lines of:
“I am only alive today because of pure chance and luck”
In most of the situations, the interviewee had been in a late stage of cancer, and by chance had stumbled upon a clinical trial that miraculously reversed their condition. In one case it was a faint suggestion online that had caused them to seek out the trial. In another it was a lucky reference from a doctor who recommended another doctor who just so happened to be studying the exact mutation of the patient. In these cases, the patient somehow managed to find a suitable trial, when the odds of finding one were close to none.
Luck should be erased from the equation of clinical trials. In other words, the recommendation that the doctor gave to visit a specialist for some disorder or the advice given on a website should not happen by chance. In an ideal setting, the right information about trials should always naturally travel to the patient. To remedy this situation, we have been designing the role of a clinical trials navigator, who will consistently provide education about trials, help patients obtain trials information. The navigator will be the person that the patient sees soon after diagnosis, and during the meeting with the navigator, the patient will be brought up to speed about clinical trials, and relevant trials will be suggested by the navigator. We hope that this will remove the chance required for patients with specific mutations who need cutting edge medicine.
Although most of the interviewees shared a similar story, some did not. One, in particular, had a completely opposite story. After being diagnosed with cancer, they immediately searched online for a possible mutations, and came to their doctor prepared with clinical trials in mind. It would be ideal if every patient acted like this, but unfortunately not every patient is so equipped. Going forth we are looking to design our solution in a way that engages not just the patients who would seek out help by themselves, but those who would not seek out aid, and are really the ones who need help the most.
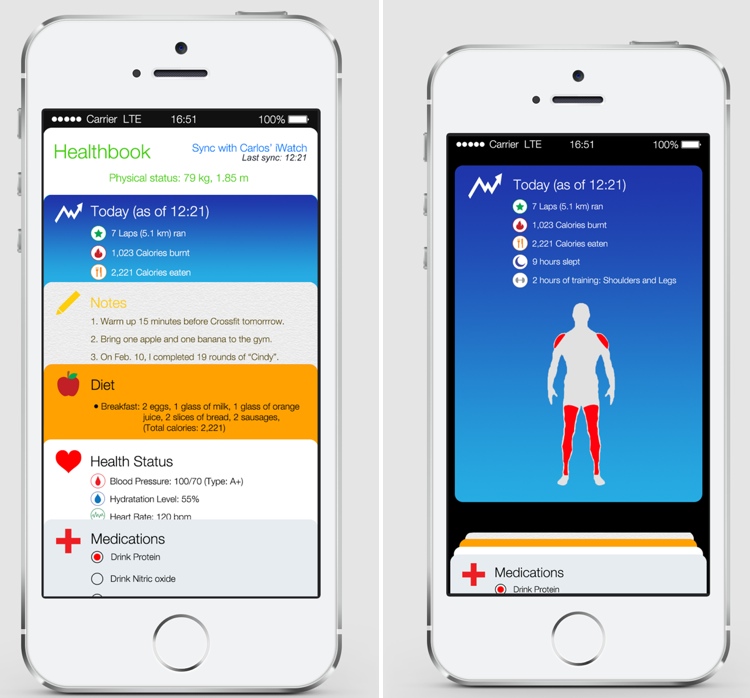
Image Source: http://farm8.staticflickr.com/7221/7175331883_80d3ebae45_b.jpg