This semester, as we’ve investigated strategies to improve inter-professional communication and care coordination in intensive care unit (ICU) rounds, I’ve been surprised by two things:
- Everyone’s seen the problem. This isn’t a situation where astute perception revealed systemic undercurrents; anyone who’s participated in rounds is intimately familiar with its inefficiencies. Everyone understands this, but nobody has definitively addressed it.
- Everyone’s thought about solutions. Whenever we’ve discussed rounds with a patient or provider, it’s profound how much they’ve given this thought. Anyone can readily suggest areas for impact, or even specific methods for improvement. Why hasn’t intuition translated to innovation?
It’s attention – or more specifically, the scarcity of it. Nobody recognizes the opportunities for creative destruction in healthcare better than the people who spend each day in the trenches of clinical medicine. But after patient care, administrative hurdles, research responsibilities, teaching duties, continuing education, and something that might resemble a personal life, providers have neither the interest nor the capacity to cultivate an innovative spirit.
Which leads me to ask: what might healthcare look like if we gave providers the time and space for disruptive thinking?
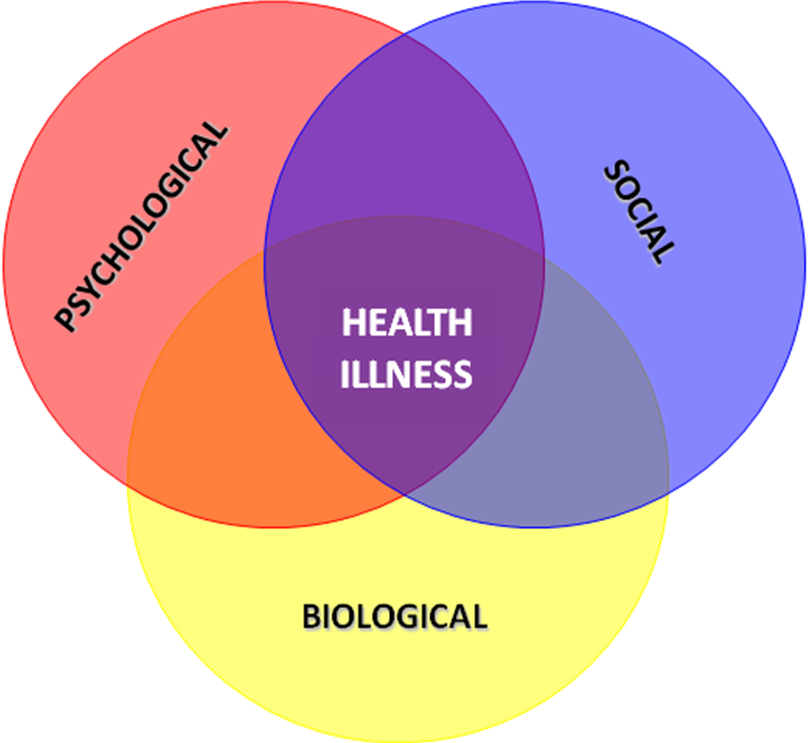
What if medical teams borrowed from Dropbox’s Hack Week? What if health institutions, as Google did, allowed every provider 20% of their time for creative ventures? What might the likes of the inventive energies and constructive cultures that created GMail, AdSense, and Google News do for healthcare? A different approach to ICU rounds? A re-designed EMR interface? A stronger capacity to screen for, and address, the social determinants of poor health? The opportunities are limitless.
And thus, for healthcare providers, students, patients, entrepreneurs, everyone, I offer these thoughts:
- What would you do if 20% of your professional time was protected for creativity and inspiration?
- In what ways does your work atmosphere cultivate innovative vision, and how could it better meet that goal?
- Beyond limits to time and attention, what are other functional obstacles to innovation in health settings, and how can we mitigate them?