Our group’s primary challenge and main research question is “How to best tell the story of Rice University and Dr. William Akers’s contribution to the development of the artificial heart in the Texas Medical Center?”.
So here are some tips from some of the nation’s best storytellers…the folks from Disney’s Pixar Animation Studios.
It may seem strange to be seeking advice from the makers of family films, but we must remember these are the guys that can take literally anything (toys, cars, rats, robots, an old man and a house full of balloons), and turn it into a story that touches the heart of people of all ages.
Thus, even though we’re not writing an original story, being able to take the information that we have and compile it into a compelling, relatable narrative will be key to making this project a success.
In 2012 storyboard artist Emma Coats (@lawnrocket) from Pixar tweeted 22 tips she wanted to impart from her time there and some folks from No Film School compiled it together into a nice list.
Among the 22 tips, here are the few that I think are most relevant to our project:
1. You gotta keep in mind what’s interesting to you as an audience, not what’s fun to do as a writer. They can be very different.
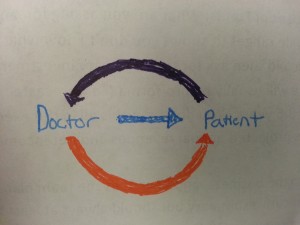
This has been another primary research question that we have been struggling with. We need to identify our audience so that we can identify what would be compelling to them. Presenting Dr. Akers’ story would be much different if we were talking to a group of biomedical engineers than if we were to a group of artificial heart patients. I think we are trying to aim for something in the middle – a story that can showcase the impressive technical designs of Dr. Akers’ work while reminding us that his contributions have served to save many lives, perhaps even lives of the people who will end up coming across this story.
7. Come up with your ending before you figure out your middle. Seriously. Endings are hard, get yours working up front.
This is a good point to make that also ties into the question, what is our ultimate goal in telling this story? Do we want it to just be historical and talk about a certain time period? Do we want to tie it back to the present? Do we want to utilize this story to call people to action? If so, what do we want our audience to do?
11. Putting it on paper lets you start fixing it. If it stays in your head, a perfect idea, you’ll never share it with anyone.
The post-it note activity we’ve been doing in class has really served this purpose. For example, in the last class we were able to brainstorm a really beautiful analogy for our project that I think will be a framework for how we are going to write the story going forward. All because we were just writing ideas on post-its.
15. If you were your character, in this situation, how would you feel? Honesty lends credibility to unbelievable situations.
16. What are the stakes? Give us reason to root for the character. What happens if they don’t succeed? Stack the odds against.
This is the part that is easier as documentary storytellers because instead of imaging the motivations of our characters we can simply ask our characters how they felt at the time – for example, when we interview Dr. Akers. In our research, we’ve begun to get a better sense of our characters’ personalities as we’ve learned a bit about what other important figures at the time, such as Dr. Liotta, thought about Dr. Akers and Dr. Akers. In terms of stakes, our problem-owner and our team were drawn to Dr. Akers when we heard that he felt unappreciated for his contribution to the design of the artificial heart, and that made him a more relatable person to which we could understand why he wanted his story to be told.But what would be the stakes for society if Dr. Akers’ story isn’t told? Who would benefit knowing more about Rice University’s involvement in the development of the artificial heart? Would current students be encouraged to pursue cardiology or biomedical engineering? Would prospective students be more likely to apply to Rice University? Would more heart patients want to be treated at the Texas Medical Center?
One idea I have moving forward is to write out the story of Dr. Akers’ and the artificial hearts as a script for a short film. Instead of primarily seeing legends such as Dr. Debakey and Dr. Akers as pioneers who I admire, I’ll write them into characters with struggles, opinions, and motivations. Being able to capture even the most basic story in an narrative form will help us see ultimately go forward with our problem session.