The following represent a rough narrative transcript of opening remarks from the Medical Futures Lab’s recent conference, Millennial Medicine – Knowledge Design for an age of Digital Disruption
The following represent a rough narrative transcript of opening remarks from the Medical Futures Lab’s recent conference, Millennial Medicine – Knowledge Design for an age of Digital Disruption
Bryan Vartabedian’s remarks
I want to welcome everyone to Millennial Medicine. My name is Bryan Vartabedian, I am a pediatrician at Baylor College of Medicine. We have a remarkable lineup of presentations that we hope you’ll find provocative and inspiring. We’ve hand selected some of the greatest visionaries and thinkers in medical education and it should be an exciting day. If you came for answers, you may be in the wrong place. Rather than offer all of the answers, we will create questions. We are hoping that Millennial Medicine will begin a new conversation about medical education.
We would like to open up by telling you a little bit about the Medical Futures Lab (MFL), the project behind this meeting. But to do that we have to offer a little background about the changes in medicine that inspired the MFL.
It seems that no matter where I turn I’m surrounded by pessimism concerning the state of our profession. Doctors are discouraged, disillusioned and under appreciated. But I happen to think that this is perhaps the most exciting time to be in medicine. Information and technology are advancing at rates faster than we can understand. Physicians are in the midst of a shift never before seen.
This has lead to something of an identity crisis for us. Everything we understand about what it means to be a doctor is changing.
We are being redefined. There are a number of forces responsible for that.
Technology – The first force pulling on us is technology. Technology has defined every medical generation before us and this generation is no differnet. A lot of what we once did with our eyes, ears and hands has been replaced. It’s been said that in the 19th century we treated symptoms, in the 20th century we treated diseases and in the 21st century we will predict, preempt and prevent disease. Clayton Christiansen calls this the move from intuitive to precision medicine.
Third party forces – Another force shaping doctors is third party control. Care is increasingly under administrative/centralized control through evidence based guidelines and information derived from big data.
Health 2.0. Perhaps the most influential force in the modern redefinition of the physician is the health 2.0 movement. Patients themselves are changing and they are, in turn, influencing us. For the better part of modern civilization our role as physician has centered around privileged access to information and knowledge. But the web has created a type of disintermediation. Patients can do more on their own. They can access information and make certain judgments. They can share information and adjust what they’re doing based on the input of others. And the physician encounter is evolving as a more narrowly defined element in an individual’s quest to understand their condition and get better. This health 2.0 element is fueled by new tools of communication and collaboration
In effect we are seeing a variety of social and technological forces conspiring to redefine the role of the physician. In the words of Eric Topol, our first speaker, we are experiencing a Creative Destruction of Medicine. We are witnessing what he calls the Great Inflection of Medicine.
But despite what Dr. Topol will so eloquently outline, we continue to see, think and work like doctors from 1957. We see medicine in a 20th century construct. And this is because in medicine, our practices and workflows are typically predicated on models shaped by the generation before us. While the physician of 2050 will think and work in a way that can only be imagined by the current generation, we are completely unprepared to deal with what lies ahead. Medical leadership and professional educators need to anticipate and study the issues evolving as medicine undergoes its most extreme transformation.
We must change how we train physicians.
And there are so many challenges
-
Our human and institutional systems for keeping pace are based on 20th century processes.
-
Real-time dialog and social transparency are blurring the boundaries between a physician’s professional and personal life
-
And, for the first time in medical history, physician trainees are more comfortable with the tools of health information and communication than their teachers.
The physician of the 21st century will need an entirely new set of literacies in order to function in this new world. These literacies must be reflected in how we train our physicians. There are many new literacies that could be identified. Here are a few:
-
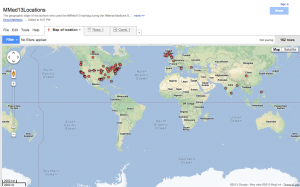
Network awareness – Within my generation we will begin to see a move from teaching doctors what they need to know to teaching them how to access what they need to know. Physicians are part of a global network, and accessing that knowledge will represent a key, new literacy.
-
Input management – Information is increasingly becoming the problem rather than the solution. Doctors need the tools and abilities to manage inputs.
-
Creation/translation of knowledge into a digital format – The translation of what we know into tagged, retrievable digital content will represent a key skill for doctors going forward.
-
Mindfulness – And despite how technical we become, we need to never allow our screens to become between us and our patients. We must train our next generation to work with technology in a way that puts the patients first.
I really believe that this is the most exciting time to be in medicine. I’m convinced I was born at just the right time in history. I was trained as an analog physician but I’m a witness to this incredible digital transformation.
Kirsten Ostherr’s remarks
Thank you. I’d like to pick up where Bryan left off by talking a bit about how we’ve designed the Medical Futures Lab to respond to some of the challenges he just laid out.
One of our core operating principles is that we are facing complex problems that require broad, multi-disciplinary collaboration among stakeholders located within and beyond medicine. As the historian of science Naomi Oreskes memorably put it in a lecture at Rice last year, “The problems of the world don’t come to us packaged in the form of academic departments.”
With this insight in mind, the Medical Futures Lab aims to overcome the silos that have traditionally separated different institutions and fields of expertise, by drawing on talent at Rice, Baylor, and the various schools of UT Health. And that talent includes both health professionals and innovative thinkers whose outsider approach to health challenges can provide the fresh perspective often needed to come up with novel solutions to old problems.
We believe that the unique challenges of practicing medicine in the digital age come from the complexity of medicine, as well as the complexity of digital media. That’s why we have formed a collaboration that brings together media scholars such as myself, along with artists and designers, to work with health professionals.
You’ll see this approach reflected in the lineup of today’s speakers, several of whom are not medical professionals, but have important things to say about the future of medical education, nonetheless.
It’s also a great tag line: As Bryan put it in a 33 charts blog post earlier this year, “An English professor and a pediatrician walk into a bar…”
The purpose of bringing this multidisciplinary team together is to train the next generation of physicians to tackle the challenges of practicing medicine in the digital age. And we believe this training requires both critical thought and media creation.
Some of the topics we’re focusing on include social media, quantified self, patient engagement, big data, mHealth, digital ethics, doctor-patient relationship, emerging technologies & health disparities.
Our approach draws on the tradition of medical humanities and infuses it with digital media theory to train our students in a field of practice we call digital medical humanities.
Our emphasis is on cultivating digital literacies – skills for optimizing health professionals’ use of digital media to improve their practice and enhance their communication with patients. And we consider education to be a lifelong engagement, so we are developing this content for all stages of medical education – from pre-med through CME.
I’ll give you a couple of brief examples of courses from this past year. ENGL 273, ENGL 278. I’m delighted to say that a number of our students – future thoughts leaders I this field – are here today, say hello! And check out their public thinking on our class tumblr. Special thank you to the Office of the Provost Faculty Initiatives Fund for their support of these classes and this symposium.
Almost half of our Rice university undergrads plan to attend medical school or go into biomedical research. So we see them as our starting point for fostering new digital literacies that they will bring with them into their medical careers. But we also see these courses as modular units that can be incorporated into medical school, residency, and beyond through online, open-access platforms. Watch the Medical Futures Lab blog for more about this in coming months!
We also believe that education transcends the traditional lecture hall setting, just as healthcare transcends the clinical setting, so I’d like to wrap up by telling you about one more of our exciting projects at the Medical Futures Lab that engages both providers and patients as 21st century active learners.
As Howard Rheingold argues in Net Smart, learning by doing is especially true when it comes to participatory media. To this end, we have created the Medical Media Arts Hub with support from the Rice University Arts Initiative Fund through the Office of the Provost. Extra special thanks to Caroline Levander for her support of this endeavor.
The Medical Media Arts Hub is an innovative online platform & media creation space where students help medical professionals amplify their health messages through creative design. Students with creative skills get to work on real communication, visualization and information problems with health professionals and patient stakeholders, getting regular feedback on the design process from engineers, creative professionals, and other members of the health community.
Health professionals get reverse mentoring from digital natives, patients actively shape their relationships with providers through the collaborative design process, and patient engagement leads to better health outcomes. Everyone wins!
We’ll be piloting our first Media Arts Hub projects this summer, so stay tuned for more as the Hub develops. Thank you for joining us for the inaugural symposium of the Medical Futures Lab. And before we turn to our first speaker, we have a brief announcement from Brian Lang, the co-founder of one of our important community partners, Health 2.0 Houston.